By Martin Li, M.A., CRCST, CER, CIS, CHL
Introduction
Data analytics has emerged as a cornerstone in modern
healthcare, transforming how decisions are made at all levels of the industry.
For Sterile Processing Departments (SPD), the integration of data analytics is
not just beneficial but essential for improving operational efficiency,
ensuring compliance, and enhancing patient safety. This article delves into the
role of data analytics in healthcare sterile processing leadership
decision-making, with a particular focus on insights from an SPD educator's perspective.
The Role of Data Analytics in Healthcare
Data analytics involves the systematic computational
analysis of data to uncover patterns, correlations, and trends that inform
decision-making. In healthcare, data analytics is used to improve patient
outcomes, streamline operations, and reduce costs. The adoption of electronic
health records (EHRs) and other digital tools has exponentially increased the
availability of data, enabling healthcare leaders to make informed decisions
based on real-time information.
Importance of Data Analytics in Sterile Processing
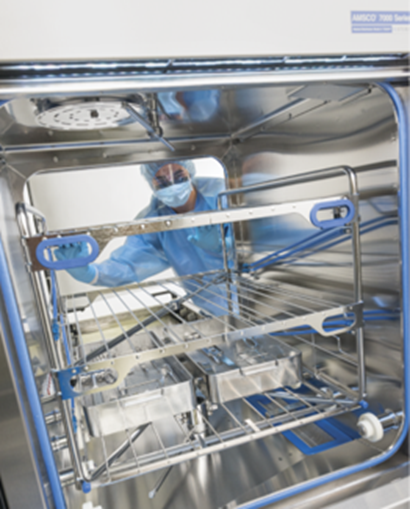
Sterile Processing Departments are critical to healthcare
facilities as they ensure that surgical instruments and other medical devices
are properly sterilized and safe for use. The complexity and high stakes
involved in SPD operations make data analytics an invaluable tool. By
leveraging data analytics, SPD leaders can enhance the efficiency of their
processes, maintain compliance with regulations, and improve overall patient
safety.
Data-Driven Decision-Making in SPD Leadership
From an SPD educator's perspective, data-driven
decision-making involves the use of data to guide leadership decisions,
identify areas for improvement, and implement evidence-based strategies. This
approach ensures that decisions are not based on intuition or anecdotal
evidence but on concrete data that reflects the actual performance and needs of
the department.
Enhancing Operational Efficiency
One of the primary benefits of data analytics in SPD is the
ability to enhance operational efficiency. By analyzing data on instrument
usage, turnaround times, and workflow processes, SPD leaders can identify
bottlenecks and inefficiencies. For instance, data might reveal that certain
instruments are consistently in high demand, leading to frequent shortages and
delays. Armed with this information, leaders can adjust inventory levels,
optimize instrument reprocessing schedules, and improve overall workflow efficiency
(Taipalus, 2023).
Ensuring Compliance and Safety
Compliance with regulatory standards is a significant
concern for SPDs. Data analytics helps ensure that all sterilization processes
adhere to the required standards and protocols. By tracking and analyzing data
on sterilization cycles, chemical indicators, and biological tests, SPD leaders
can quickly identify and address any deviations from established protocols,
thereby ensuring compliance and maintaining patient safety (Reed, 2024).
Predictive Maintenance and Equipment Management
Data analytics also plays a crucial role in predictive
maintenance and equipment management. By analyzing data on equipment
performance and maintenance history, SPD leaders can predict when equipment is
likely to fail and schedule preventive maintenance accordingly. This proactive
approach reduces downtime, extends the lifespan of equipment, and ensures that
critical devices are always available when needed.
Implementing Data Analytics in SPD: Challenges and
Solutions
While the benefits of data analytics in SPD are clear,
implementing these systems can be challenging. Common challenges include data
integration, staff training, and ensuring data quality. From an SPD educator's
perspective, addressing these challenges involves a multifaceted approach.
Data Integration
Integrating data from various sources, such as EHRs,
sterilization records, and inventory management systems, can be complex.
Effective data integration requires robust IT infrastructure and
interoperability between different systems. Educators play a crucial role in
facilitating this process by collaborating with IT professionals to ensure that
data flows seamlessly across platforms.
Staff Training
For data analytics to be effective, SPD staff must be
proficient in using data-driven tools and interpreting analytical reports.
Educators are responsible for designing and delivering comprehensive training
programs that equip staff with the necessary skills. This includes training on
data entry, data interpretation, and the use of specific analytics software.
Ensuring Data Quality
The accuracy and reliability of data are paramount in
data-driven decision-making. Educators must emphasize the importance of
accurate data entry and implement regular audits to ensure data quality. This
involves setting up standardized procedures for data collection and entry, as
well as conducting periodic reviews to identify and correct any discrepancies.
Case Study: Data Analytics in Action
To illustrate the practical application of data analytics in
SPD leadership, consider a case study of a mid-sized hospital that implemented
a data-driven approach to improve its sterile processing operations.
Background
The hospital faced challenges with instrument availability
and reprocessing efficiency. Frequent delays in instrument turnaround times led
to surgical schedule disruptions and increased costs. The SPD leadership
decided to adopt a data analytics solution to address these issues.
Implementation
The first step was to integrate data from the hospital's
EHR, sterilization records, and inventory management system. This integration
provided a comprehensive view of instrument usage, reprocessing cycles, and
equipment performance. The hospital also invested in training its SPD staff on
data analytics tools and techniques.
Results
Within six months of implementation, the hospital saw
significant improvements in its SPD operations. Data analysis revealed that
certain instruments were being underutilized while others were overused. By
adjusting inventory levels and reprocessing schedules, the hospital reduced
instrument shortages and turnaround times by 30%. Additionally, predictive
maintenance data helped the hospital avoid unexpected equipment failures,
further enhancing efficiency and reducing costs.
The Future of Data Analytics in SPD
The future of data analytics in SPD is promising, with
advancements in technology continually expanding the possibilities. Emerging
technologies such as artificial intelligence (AI) and machine learning (ML) are
expected to further enhance the capabilities of data analytics in healthcare.
Artificial Intelligence and Machine Learning
AI and ML can analyze vast amounts of data more quickly and
accurately than traditional methods. In SPD, these technologies can be used to
predict instrument demand, optimize reprocessing schedules, and identify
potential equipment failures before they occur. AI-driven analytics can also
assist in identifying patterns and trends that might not be immediately
apparent through manual analysis.
Real-Time Data Analytics
Real-time data analytics is another emerging trend that
holds great potential for SPD. By providing real-time insights into instrument
usage and reprocessing status, SPD leaders can make immediate adjustments to
their operations. This can lead to more responsive and agile decision-making,
further improving efficiency and patient safety.
Conclusion
Data analytics is a powerful tool that can significantly
enhance decision-making in healthcare sterile processing departments. From an
SPD educator's perspective, the integration of data analytics involves not only
the adoption of new technologies but also the development of skills and
processes that ensure effective data-driven decision-making. By addressing
challenges such as data integration, staff training, and data quality, SPD
leaders can leverage data analytics to improve operational efficiency, ensure
compliance, and enhance patient safety. As technology continues to advance, the
role of data analytics in SPD will only grow, offering even greater
opportunities for innovation and improvement in healthcare.
References
- Taipalus,
T. (2023). Data Analytics in Healthcare: A Tertiary Study. PMC. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9734338/
- Reed,
B. (2024). 3 Ways Big Data Will Ensure your Sterile Processing. LinkedIn. https://www.linkedin.com/pulse/3-ways-big-data-ensure-your-sterile-processing-department-brian-reed
- Data-Driven
Decision-Making for Health Administrators. (2022). Tulane University. https://publichealth.tulane.edu/blog/data-driven-decision-making/
- Reference
examples - APA Style. (n.d.). APA Style. https://apastyle.apa.org/style-grammar-guidelines/references/examples
- Citing
Sources: APA Citation Examples. (2024). WPI. https://libguides.wpi.edu/citingsources/apa_examples
- In-Text
Citations: Author/Authors. (n.d.). Purdue OWL. https://owl.purdue.edu/owl/research_and_citation/apa6_style/apa_formatting_and_style_guide/in_text_citations_author_authors.html