https://www.steris.com/healthcare/knowledge-center/
Surgical instruments and other reusable devices must be
effectively reprocessed so they are safe and functional for patient use. Before
an instrument can go through sterilization or high-level disinfection, it must
be cleaned. To ensure quality outcomes for the patient, the cleaning process
requires consistency and standardization.
Before reviewing the details of the process, it's important
to understand the distinction between "cleaning" and
"disinfection." Here are a few key definitions to know:
- Visible Soil: Blood, bone, tissue, and
inorganic soils such as dirt or dust
- Non-Visible Soil: Microorganisms, bacteria,
and viruses or chemicals
- Cleaning/Decontaminating: The removal of
contamination (often referred to as "soil") from a surface to
the extent necessary for further reprocessing or the intended use of the
surface. (ANSI/AAMI/ISO 15883-1)
- Disinfection: The antimicrobial reduction
of the number of viable microorganisms on a product or surface to a level
previously specified as appropriate for its intended further handling.
Most automated washer/disinfectors will accomplish this through thermal
disinfection.
- High Level Disinfection: The elimination of all
microorganisms in or on an instrument, except for small numbers of
bacterial spores.
- Sterilization: The process to eliminate
all viable microorganisms.
Next, let's review the steps in reprocessing surgical
instruments starting from point-of-use to manual cleaning and finally automated
cleaning using a washer/disinfector or ultrasonic cleaner.
STEP
1: POINT OF USE PRE-CLEANING
The first step in cleaning a surgical instrument is to
initiate pre-treatment. Instrument transport gels, like Pre-Klenz™ Point
of Use Preprocessing Gel, help initiate the cleaning process of
surgical, endoscopic, and robotic instruments immediately after use. Instrument
transport gels prevent the drying of bioburden, which can decrease the time
needed to manually clean the sink, as well as loosen soils.
STEP
2: MANUAL CLEANING OF SURGICAL INSTRUMENTS
After point-of-use pre-cleaning, instruments are
transported to the decontamination area of the Sterile Processing Department
(SPD) to begin manual cleaning. Manual cleaning should
be performed on all instruments but may be recommended as the preferred method
of cleaning for delicate or complex devices, such as endoscopes or
microsurgical instruments. Devices must be removed from the transportation
container and disassembled to expose all the surfaces to the cleaning process.
Always follow the device's Instructions for Use (IFU) for comprehensive
instructions for cleaning and disassembly.
For manual cleaning, a three bay sink
configuration is recommended. When using a three bay
configuration:
- The first sink bay will have instruments being pre-rinsed with cold
water to remove any pre-treatment product or blood.
- The second bay will have instruments immersed and pre-soaking in an
enzymatic or neutral detergent solution, then manually brushed using instrument
cleaning brushes. When a manufacturer’s IFU recommends
immersion of the device, cleaning in the sink should be done under the
water line to prevent exposure to microorganisms and aerosol generation,
especially when brushes are used to clean lumens. The cleaning
detergent should be low-foaming so staff can see clearly
into the sink to identify all instruments and prevent injuries from sharp
objects.
- The third sink bay is used for the final treated rinse. Depending on
the manufacturer’s recommended practices or a facility’s standards, the
final rinse water should be of a certain quality to help reduce any risk
to a patient of a device. Examples include controlled levels of water
hardness (to prevent spotting), chloride (to prevent device damage) and
microorganisms (to prevent cross-contamination).
STEP
3: AUTOMATED WASHING AND DISINFECTION OF SURGICAL INSTRUMENTS
After manual cleaning, most devices are then processed
through automated cleaning technologies such as ultrasonic cleaning systems and
washer/disinfectors.
Ultrasonic Cleaning
Ultrasonic cleaning is used for fine cleaning of
instruments with hard-to-reach areas like crevices, hinges, and lumens. After
manual cleaning, the devices should be sorted based on metal to prevent damage.
For example, aluminum instruments can react with stainless steel if immersed
together, causing etching, or replating to the devices.
Ultrasonic
cleaners work through cavitation where high-frequency sonic
waves create tiny bubbles on the surfaces of the instruments which eventually
implode. The implosion of these bubbles helps to dislodge soil from the surface
of the device. Low-foaming enzymatic cleaners can be used in ultrasonic
cleaners, assuming the foam does not interfere with the cavitation process.
After the ultrasonic
cleaning process, the instruments must be thoroughly rinsed with
either deionized or softened water.
Advantages of ultrasonic cleaning include a reduction of
time spent to clean complex instruments and removal of residual soil, however
not all materials or devices are compatible with this type of cleaning.
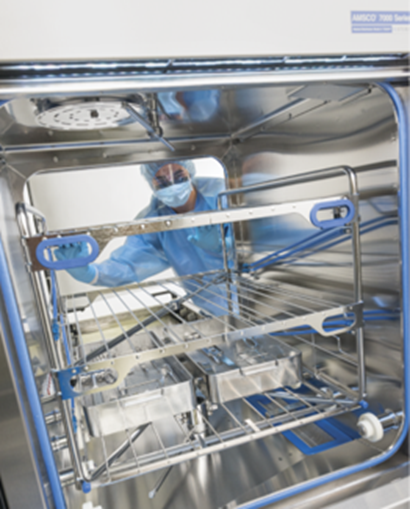
Washer/Disinfectors
The mechanical cleaning action of washer/disinfectors
relies on spray arm technology with pressurized water to help clean surgical
instruments or other reusable devices. The load inside a washer/disinfector is
exposed to a specific water temperature, chemical concentration, and flow rate.
The thermal rinse phase in a washer/disinfector provides a level of
disinfection. An optional drying phase can be added to reduce manual drying.
Successful cleaning using washer/disinfectors depends on
four parameters within the cycle:
- Time – If the cycle is too short, cleaning may not be achieved;
however, if it's too long, efficiency is compromised.
- Temperature – The temperature of the cycle wash depends on the
validated pre-programmed cycle and cleaning chemistries being used.
• When
enzymatic cleaning chemistries are used in washer/disinfectors, they typically
work best between 100-140 F/32-60 C with detergents typically being used in
ranges between 122-180 F/50-82 C. This can vary by manufacturer.
- Chemistry – The recommended cleaning chemistries are determined by
the washer/disinfector manufacturer and the IFUs for the devices being
processed. Other factors to consider in selecting a cleaning chemistry are
water quality and concentration of chemistry.
- Impingement – Representative of the mechanical force of spray arms.
If low impingement washer/disinfectors are used, a more aggressive
cleaning chemistry may be needed. High impingement washers rely on the
high pressure of the water to aid in soil removal.
Washer/disinfector
cleaning offers consistency and productivity, as parameter
control is easier. Staff must be properly trained on device loading to ensure
effective use.
CLEANING
FAILURES – RESIDUAL SOIL AND COMMON CAUSES
If after manual and mechanical cleaning soil is still
present, this can present several risks, with the most severe being the risk of
transmission to patients. In addition, residual soils left on devices can
damage the device's surfaces or ability to function correctly.
Possible Causes of Cleaning Failures
If soils are left on surgical instruments or reusable
devices after cleaning, common causes could be:
- Ineffective use of cleaning chemistries – Either the wrong chemistry
was used or an incorrect dilution rate
- Assembly of the instrument – The instrument was disassembled
incorrectly, which caused soils to become stuck in crevices or lumens
- Issues or failures with equipment – Problems with the mechanical
technologies, including misuse (i.e. overcrowding of trays) or equipment
failures
- Issues with manufacturer instructions – Instructions are either hard
to follow or contradict department procedures
CLEANING
VERIFICATION AND INSPECTION METHODS
After cleaning, all devices should be visually inspected
thoroughly with a lighted magnifying glass. In addition to routine visual
inspection, there are several methods that can be used to test cleaning
efficacy:
- Cleaning Indicators – Cleaning
process indicators verify that the washer/disinfector
cycle process parameters in all phases have the cleaning cycle have been
achieved. The indicator materials will break down or exhibit a color
change when the parameters have been successfully achieved.
- Cleaning
Verification – Beyond visual inspection, many hospitals
use a cleaning verification program such as ATP or Protein detection.
Protein is found in almost all surgical soils, and any living organism,
therefore detecting it on a "clean" device can help identify
gaps in cleaning procedures or hidden damage to devices.
GUIDELINES
FOR CLEANING AND DISINFECTING SURGICAL INSTRUMENTS
There are a variety of standards surrounding cleaning
surgical instruments and medical devices. Governing agencies, including
AAMI/ANSI, FDA, and AORN release guidelines for cleaning and disinfection.
Specific device IFUs should always be followed to ensure the device is
reprocessed according to the manufacturer. The specific standards/guidelines
around cleaning are spread throughout many standards, but the most common ones
are:
- ANSI/AAMI ST79, Comprehensive guide to
steam sterilization and sterility assurance in health care facilities –
most commonly referenced because of its detailed washer indicator
Appendix.
- ANSI/AAMI ST58, Chemical Sterilization
and High-Level Disinfection in Health Care Facilities
- ANSI/AAMI ST91, Flexible and Semi-Rigid
Endoscope Processing in Health Care Facilities – because of its
focus on the cleaning of complex endoscopy devices
IMPORTANCE
OF PROPERLY CLEANING REUSABLE DEVICES
Cleaning is an important step in the reprocessing of a
reusable device or surgical instrument. Both manual and automated cleaning can
be used and the methods will vary based on the device. Cleaning reusable
devices is important to prevent what we can see – including device damage – as
well as what we can't see like pathogenic microorganisms or transmissible
proteins. If devices are not clean, they cannot be properly sterilized, or
high-level disinfected.








No comments:
Post a Comment